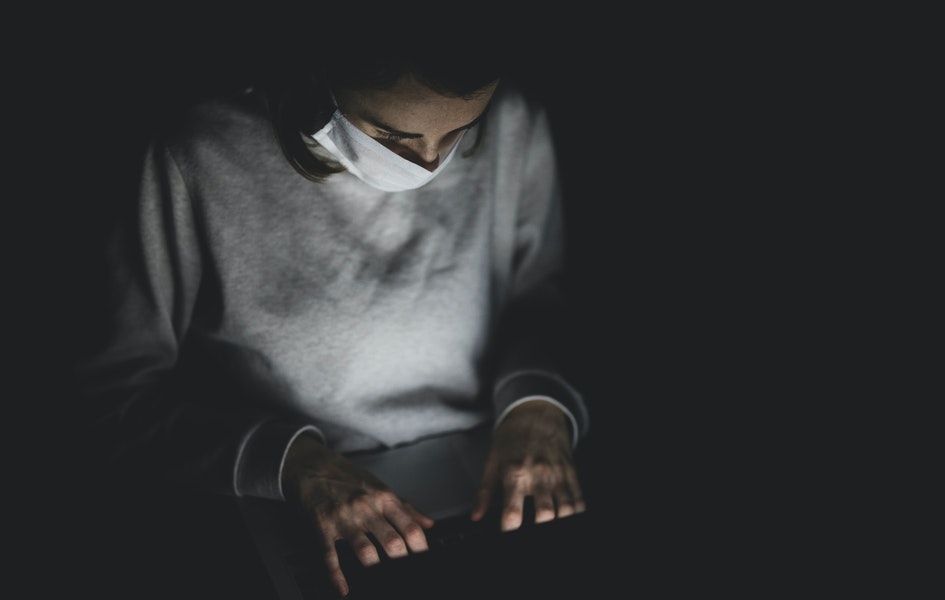
Telemedicine is becoming increasingly popular in this era of the pandemic. This integration of cameras, computer networks, software, and display technology has the potential to transform the medical profession and have a profound impact on patients' lives.
Telemedicine not only connects patients and medical providers, but it also allows health care workers to consult with other physicians or specialists in the diagnosis or treatment of a patient without leaving their facilities.
But it has its limitations.
Limitations of Telemedicine
One of the basics of medicine includes a physical exam. New technologies and techniques are developed in medicine every year, making it a continually growing discipline. With the development of more sensitive tests, clinicians have started doubting the sensitivity of physical exams; when compared to modern medicine modalities.
Physicians mustn't lose sight of the core of their physical exam abilities, which begins with inspection during these times of social separation and limiting virus exposure.
Several case studies show that in covid times, patients have been uncomfortable with removing their clothes for a thorough body checkup. Even physicians have not forced them to do so and e-consulted them to limit exposure and preserve PPE, eliminating the physical exam. Although these are vital precautions, they may increase the risk of missing physical exam findings critical to a correct and prompt diagnosis in one-of-a-kind cases.
There have been many cases in which a patient has been prescribed a treatment upon initial checkup. But when that treatment was rendered ineffective, they were treated again after a full-body checkup. Physicians found new critical pieces of evidence for treating such patients thereafter.
In this era of modern medicine, It can be challenging to stick to the fundamentals of medicine. But when the opportunity arises, a comprehensive physical exam is critical for accurate clinical diagnosis and better patient outcomes.
The above-discussed case demonstrated the adverse effects of over-dependence on technology.
Adapting to a new Technology
Next up, we shall discuss the hospital settings which take time to adapt to new technologies. If you build it, they will come does not apply to clinical systems. Every year, a multimillion-dollar clinical system blunder makes headlines. Many of those failures can be ascribed to physicians and nurses refusing to use the system. Though, they are not to be blamed entirely.
The technology involved is frequently cumbersome, difficult to understand, or incompatible with the existing patient care process. These challenges become more complicated when a system is over budget and a year or more late.
Several factors help smoothen the technology adoption process. Some of which are:
The hospital setting should be ready to adopt that new technology to foray into modern healthcare and tap into new opportunities.
Before the final implementation, all the healthcare professionals involved should get a hands-on demo of the product. Once they are completely comfortable and all their queries have been resolved, the implementation shall begin.
The adoption of new technology should not increase the workload; but rather help in reducing it. Many a time, the exact opposite happens.
The right timing is critical. We need to make sure that the technological mindset of HCPs in a hospital setting is somewhat close to that of the product.
Following these steps can help with the technology adoption process and reap the benefits of modern medicine.
In-State vs Out-State Providers
Third in our discussion is the rise in fraud, potential access problems for vulnerable groups, and conflicts between out-of-state and in-state health providers due to telemedicine.
In-state physicians are concerned that an inflow of out-of-state providers may cause them to lose a considerable chunk of their privately insured patients.
Meanwhile, telehealth fraud cases have gone through the roof. Many fraudsters are trying to steal the identities of patients and sell them on the black market. Some providers are overcharging. A while back, some fraudsters offered to put patients onto the front line covid vaccines in exchange for a payment!
You will find the pros of telemedicine plastered all over the internet, but we wanted to make sure that you know the challenges associated with it too. We hope you will find it valuable in your modern healthcare journey.
If you would like to discuss more, you can join our panel to discuss and collaborate with your like-minded peers. Join our global online community of healthcare professionals here - https://us.mymedicalpanel.com/ to learn, collaborate, discuss, and much more!
Want to learn more about us? We have answered some of the most frequently asked questions about us below, but you can always reach our global team at support@mymedicalpanel.com for any question/suggestion/feedback.
FAQs
What is My Medical Panel?
My Medical Panel (MMP) is a global online community of healthcare professionals from 150+ domains committed to aiding the medical field through healthcare market research studies.
How can I Join My Medical Panel?
Please click on the Join Us button on our website and fill in the requested information. You will be receiving a confirmation via email/phone call to confirm the details you have shared.
Is there any subscription or membership fee?
No, there is no subscription or membership fee. Instead, we provide incentives in the form of honorarium when you participate in our research studies.